Table of Contents
Overview
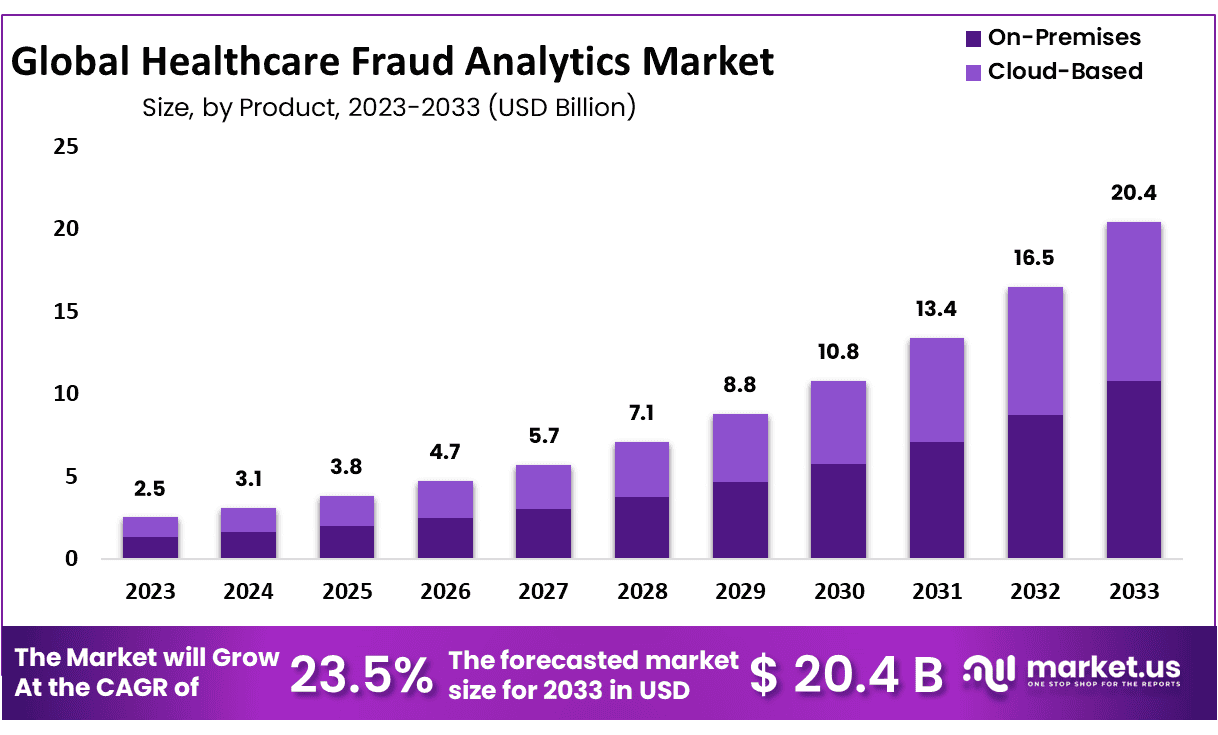
New York, NY – Sep 18, 2025 – The Global Healthcare Fraud Analytics Market size is expected to be worth around USD 20.4 Billion by 2033 from USD 3.1 Billion in 2024, growing at a CAGR of 23.5% during the forecast period from 2025 to 2033.
The adoption of Healthcare Fraud Analytics is gaining significant momentum as healthcare providers, insurers, and regulators intensify their focus on fraud detection and prevention. The technology is designed to analyze vast volumes of claims, billing records, and patient data, enabling organizations to identify irregular patterns, reduce financial losses, and ensure compliance with regulatory frameworks.
The global burden of healthcare fraud has been rising steadily, costing the industry billions of dollars annually. This has led to the rapid deployment of advanced analytics platforms powered by artificial intelligence, machine learning, and predictive modeling. These tools allow healthcare stakeholders to detect fraudulent practices in real time, minimizing risks and enhancing overall system efficiency.
Healthcare Fraud Analytics not only reduces costs but also strengthens patient trust by safeguarding resources and ensuring ethical medical practices. Key applications include claims review, prescription monitoring, provider profiling, and patient identity verification. Growing investment in digital health infrastructure and stricter regulatory requirements are further accelerating the market expansion.
North America currently leads adoption due to well-established healthcare systems and the presence of leading technology providers. However, emerging economies in Asia-Pacific and Latin America are expected to witness robust growth as governments adopt digital transformation initiatives.
With the rising need for transparency, accountability, and cost efficiency, Healthcare Fraud Analytics is poised to become an indispensable component of modern healthcare management, ensuring sustainability and fairness across the sector.
Key Takeaways
- Market Size & Growth: The Healthcare Fraud Analytics market was valued at USD 2.5 billion in 2023 and is projected to reach approximately USD 20.4 billion by 2033, registering a compound annual growth rate (CAGR) of 23.5%.
- Type Analysis: Descriptive analytics accounted for the largest share of the market, representing nearly 41.2% of total revenue in 2023.
- Delivery Model Analysis: In terms of delivery models, the on-premise segment led the market in 2023, capturing 52.9% of the overall revenue share.
- Application Analysis: By application, insurance claims review emerged as the dominant segment in 2023, contributing more than 36.5% to the market.
- End-Use Analysis: Public and government agencies were the leading end-users of healthcare fraud analytics in 2023, representing over 40.8% of market share.
- Regional Analysis: North America remained the largest regional market, accounting for approximately 37.8% of global revenue in 2023, equivalent to USD 0.945 billion.
- Healthcare Fraud Analytics Demand: The demand for healthcare fraud analytics continues to rise as organizations confront growing risks associated with fraudulent activities in healthcare services.
- Technological Advancements: Advances in artificial intelligence (AI) and machine learning (ML) are enhancing the accuracy, efficiency, and adaptability of fraud detection systems, driving continuous innovation across the market.
Healthcare Fraud Analytics Technical Analysis
Healthcare fraud analytics involves the application of advanced data science techniques to detect, prevent, and investigate fraudulent activities in healthcare systems. Large datasets from claims, electronic health records, and billing systems are analyzed using predictive modeling, anomaly detection, and machine learning algorithms.
The objective is to identify unusual patterns such as excessive billing, duplicate claims, or unnecessary procedures that indicate potential fraud. Risk scoring and real-time monitoring enable proactive detection, while natural language processing (NLP) is increasingly used to analyze unstructured clinical notes for inconsistencies.
Technical frameworks rely on big data platforms, cloud infrastructure, and AI-powered analytics to handle high data volumes efficiently. Integration with visualization dashboards and automated alerts enhances decision-making for insurers, providers, and regulators. The adoption of fraud analytics not only minimizes financial losses but also improves operational efficiency and safeguards patient trust in healthcare delivery.
Regional Analysis
North America accounted for approximately 37.8% of the global healthcare fraud analytics market in 2023, generating USD 0.945 billion in revenue. This dominance can be attributed to several factors, including high per capita income, significant healthcare spending, and widespread health insurance coverage among an aging patient population.
The rising incidence of healthcare fraud, coupled with strong government initiatives aimed at combating fraudulent practices and reducing healthcare costs, has further supported market growth in the region. Additionally, the presence of numerous service providers and continuous advancements in fraud detection software have contributed to market expansion.
The region also benefits from the presence of leading industry players. For instance, International Business Machines Corporation (IBM), headquartered in Armonk, New York, plays a pivotal role in driving demand for advanced fraud detection solutions.
However, certain challenges persist. According to findings by the U.S. Department of Health and Human Services (HHS) in 2018, flaws in national Medicaid data create significant barriers to effective fraud detection within the public sector. The Office of Inspector General (OIG) has noted that Medicaid data often suffers from inaccuracies and incompleteness, hindering the identification of fraudulent claims. These shortcomings result in billions of dollars lost annually due to fraud and abuse, posing a restraint on the overall market growth.
Frequently Asked Questions on Healthcare Fraud Analytics
- What is healthcare fraud analytics?
Healthcare fraud analytics refers to the use of advanced data analysis techniques, including predictive modeling, machine learning, and data mining, to identify, detect, and prevent fraudulent claims, billing irregularities, and abuse in healthcare systems and insurance. - How does healthcare fraud analytics work?
The system works by analyzing structured and unstructured healthcare data, identifying unusual patterns or anomalies in claims, prescriptions, or billing activities, and generating alerts for further investigation. It integrates historical data, risk scoring, and predictive models to reduce fraud. - Why is healthcare fraud analytics important?
Healthcare fraud analytics is important because it reduces financial losses, improves compliance, and enhances patient safety. By detecting fraudulent claims early, healthcare providers and payers can save billions of dollars and ensure resources are used for genuine care. - What technologies are used in healthcare fraud analytics?
Key technologies include artificial intelligence (AI), machine learning (ML), big data analytics, natural language processing (NLP), and predictive modeling. These technologies allow continuous monitoring of healthcare data and proactive detection of fraudulent practices with higher accuracy and speed. - Who uses healthcare fraud analytics?
Users include government agencies, healthcare insurance providers, hospitals, pharmacies, and private payers. These stakeholders rely on fraud analytics to strengthen compliance frameworks, protect financial integrity, and maintain transparency across healthcare claims and reimbursement processes.
Use Cases
- Claim Pattern Anomaly Detection
- Description: Detect abnormal patterns in submitted claims that deviate significantly from expected norms. For example, a provider suddenly billing much more than peers, or submitting unusually high volumes of certain high-cost procedures.
- How analytics is used: Statistical models or machine learning detect outliers; clustering or unsupervised learning may flag providers whose billing patterns diverge from peer group or historical behavior.
- Evidence/Data: The U.S. Department of Health & Human Services (HHS) uses machine learning on Medicare & Medicaid claims data to identify new emerging fraud, waste, and abuse cases beyond just known fraud schemes.
- Impact: In the 2025 U.S. National Health Care Fraud Takedown, 324 defendants across many provider types were charged for schemes with intended losses above US$ 14.6 billion. Many of these frauds were identified via claims analysis.
- Preventing Payment of False or Fraudulent Claims Before Disbursement
- Description: Before paying out claims, the system evaluates requests to see if they are likely false or fraudulent. If detected, payments are delayed or denied.
- Analytics role: Use predictive models, rule-based systems, and fraud risk scores. Also, real-time flagging systems to prevent payment.
- Evidence/Data: In the same 2025 U.S. fraud takedown, the Centers for Medicare & Medicaid Services (CMS) succeeded in preventing over US$ 4 billion from being paid in response to false or fraudulent claims.
- Provider Behavior Monitoring for Emerging/Unseen Fraud Schemes
- Description: Monitoring providers for behaviour that does not match past known fraud but is suspicious—this helps in catching new/evolving fraud tactics (e.g., new types of upcoding, new billing combinations).
- Analytics role: Use unsupervised learning, anomaly detection, deep learning, change detection (difference from baseline) etc. Also, periodic audits triggered by unusual trends.
- Evidence/Data: HHS is developing fraud, waste, and abuse (FWA) models that do *notrely solely on past known schemes; using tree-based models + deep learning to assign weights to features in Medicare/Medicaid claims.
- Investigation Prioritization & Resource Allocation
- Description: Given limited investigative resources, analytics helps in prioritizing which cases or providers to investigate first (i.e., those with highest risk or highest potential loss). This ensures resources are used most effectively.
- Analytics role: Risk scoring of providers, segmentation by potential loss, combining multiple indicators (e.g., past infractions, high billing amounts, types of services, geographic region).
- Evidence/Data: The HHS project (from “Artificial Intelligence: Select Use Cases” PDF) describes a “Unified Case Management” system acting as centralized repository and workflow to coordinate investigations; with alerting of likely fraud schemes so investigators can prioritize.
- Law Enforcement Collaboration & Large-Scale Fraud Takedowns
- Description: Multi-agency efforts to detect, prosecute, and stop major fraud schemes that affect large numbers of providers and large sums. Analytics supports these by aggregating data, spotting networks, linking providers, supply chains, billing entities.
- Analytics role: Network analysis, linking data across states/programs, identity matching, detection of straw-owners or fake entities, pattern recognition across jurisdictions.
- Evidence/Data: The 2025 National Health Care Fraud Takedown: 324 defendants were charged, including 96 medical professionals, for fraud involving over US$ 14.6 billion in intended loss. Over $ 245 million in assets (cash, luxury vehicles, cryptocurrency, etc.) were seized.
Conclusion
The adoption of healthcare fraud analytics is transforming the healthcare industry by enabling real-time detection, prevention, and investigation of fraudulent activities. With advanced technologies like AI, machine learning, and predictive modeling, stakeholders are effectively reducing financial losses, ensuring regulatory compliance, and safeguarding patient trust.
The market’s rapid growth projected to reach USD 20.4 billion by 2033 reflects rising global awareness and investment in digital health security. As fraud schemes become more complex, healthcare fraud analytics will remain a critical tool in enhancing transparency, operational efficiency, and ethical practices across healthcare systems worldwide. Its strategic value is now indispensable for sustainable healthcare management.


